
Because circulating 25(OH)D was insufficient in 25% of those patients, i.e. We have characterized cross-sectional relationships between vitamin D intakes, 25(OH)D, 1,25(OH) 2D and PTH in endocrine outpatients. Vitamin D consumption in the amount of 100 mcg (4000 IU)/day is safe and physiologic for adults. Resistance from manufacturers may also stem from the fact that no clinical study has yet specifically used 15 mcg (600 IU)/day of vitamin D 3.

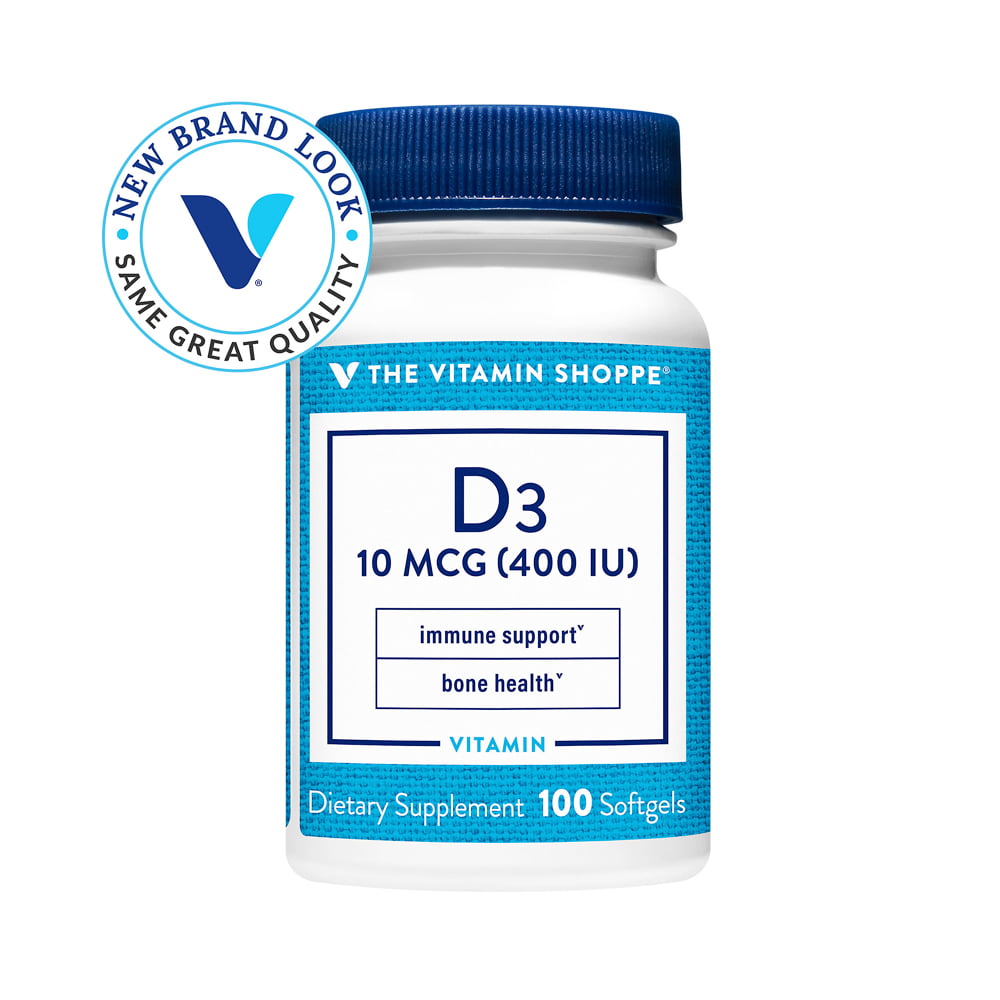
Controversies and ongoing concerns about exceeding the safe upper limit (UL) for vitamin D are probably why every major brand of multivitamins marketed for older adults still contains less than the adequate intake (AI) for adults >70 y. According to this criterion, there is still no scientific basis for an RDA for vitamin D. A recommended dietary allowance (RDA) is an intake "adequate to meet the known nutritional needs of practically all healthy persons". For osteoporosis prevention, the recent consensus is that 25(OH)D should exceed 72 nmol/L, and that adult consumption of vitamin D should be about 25 mcg (1000 IU)/day. Vitamin D nutrition can affect many aspects of health because its metabolites function at many tissues. This work confirms the safety and efficacy of both 15 and 100 mcg/day vitamin D 3 in patients who needed additional vitamin D. Since it was ethically necessary to provide a meaningful dose of vitamin D to these insufficient patients, we cannot rule out a placebo wellbeing response, particularly for those on the lower dose. The 100 mcg/day dose produced greater responses. In Study 1, 64 outpatients (recruited if summer 2001 25(OH)D 40 nmol/L, lowered PTH, and its use was associated with improved wellbeing.

We compared effects of these doses on biochemical responses and sense of wellbeing in a blinded, randomized trial. The adequate intake (AI) for older adults is 15 mcg (600 IU)/day, but there has been no report focusing on use of this dose. For adults, vitamin D intake of 100 mcg (4000 IU)/day is physiologic and safe.


 0 kommentar(er)
0 kommentar(er)
